More Than Just "Cysts on Your Ovaries"
Polycystic Ovary Syndrome (PCOS) is the most common hormonal disorder in women of reproductive age, affecting 8-13% of women. Yet it's also one of the most misunderstood and poorly treated conditions.
First, the name is misleading. You don't need cysts to have PCOS, and having cysts doesn't mean you have PCOS. The "cysts" are actually immature follicles that never developed enough to ovulate—a consequence of the hormonal dysfunction, not the cause.
Second, PCOS isn't a single disease with a single cause. It's an umbrella diagnosis that can result from several different underlying mechanisms. Treating all PCOS the same way is why so many women don't get better.
How PCOS Is Diagnosed
The Rotterdam criteria (most widely used) require 2 of 3 features:
Irregular or Absent Ovulation
Cycles longer than 35 days, fewer than 8 periods per year, or no periods at all.
High Androgens
Either elevated testosterone/DHEA on labs OR clinical signs like acne, hirsutism (male-pattern hair growth), or hair loss.
Polycystic Ovaries on Ultrasound
12+ follicles per ovary or ovarian volume >10mL. (Note: Up to 25% of normal women have polycystic-appearing ovaries.)
Important: Other conditions that cause similar symptoms must be ruled out first—thyroid disease, hyperprolactinemia, congenital adrenal hyperplasia, and Cushing's syndrome.
The Different Types of PCOS
This is where most treatment fails. A woman with insulin-resistant PCOS needs different interventions than one with adrenal PCOS or post-pill PCOS. Here are the main types:
1. Insulin-Resistant PCOS
The most common type (70% of cases). High insulin drives the ovaries to produce excess androgens and disrupts ovulation. Often associated with weight gain, but can occur in lean women too.
Signs & Labs
- • Elevated fasting insulin (>10 μIU/mL)
- • High triglycerides, low HDL
- • Acanthosis nigricans (dark skin patches)
- • Weight concentrated around midsection
- • Sugar/carb cravings
Key Interventions
- • Blood sugar management (diet, exercise)
- • Metformin or inositol
- • Strength training
- • Weight loss (if overweight)
- • GLP-1 medications in some cases
2. Adrenal PCOS
About 20-30% of cases. Elevated DHEA-S (an adrenal androgen) with normal testosterone. Often driven by stress and HPA axis dysfunction rather than insulin.
Signs & Labs
- • Elevated DHEA-S, normal testosterone
- • Normal insulin and metabolic markers
- • Often lean body type
- • History of chronic stress
- • Wired-but-tired feeling
Key Interventions
- • Stress reduction (critical)
- • Adequate sleep
- • Adaptogenic herbs (ashwagandha)
- • NOT aggressive dieting/fasting
- • Sometimes low-dose cortisol support
3. Inflammatory PCOS
Chronic inflammation drives androgen production and disrupts ovulation. Often overlaps with insulin resistance, but inflammation is the primary driver.
Signs & Labs
- • Elevated hsCRP
- • Skin issues (eczema, rashes)
- • Digestive issues, IBS
- • Joint pain, headaches
- • Fatigue disproportionate to other labs
Key Interventions
- • Anti-inflammatory diet
- • Gut health optimization
- • Identify food sensitivities
- • Omega-3s, turmeric
- • Address environmental toxins
4. Post-Pill PCOS
Temporary PCOS-like symptoms after stopping hormonal birth control. The pill suppresses your own hormone production; it can take time for normal cycling to resume.
Signs
- • Regular cycles before the pill
- • PCOS symptoms only after stopping
- • Often resolves within 3-12 months
- • May have elevated LH:FSH ratio
- • Usually no insulin resistance
Key Interventions
- • Time (often resolves on its own)
- • Support ovulation recovery
- • Zinc, B vitamins
- • Avoid rushing back to the pill
- • Cycle tracking to monitor recovery
The PCOS Hormone Pattern
Understanding the hormonal cascade helps explain why symptoms cluster together:
High LH, Low/Normal FSH
The LH:FSH ratio is often elevated (2:1 or higher). High LH stimulates the ovaries to produce androgens. Low FSH means follicles don't mature properly for ovulation.
Elevated Androgens
Total testosterone, free testosterone, and/or DHEA-S may be elevated. This causes acne, hirsutism, and hair loss. It also disrupts the normal follicle development.
Low Progesterone
Without ovulation, there's no corpus luteum to produce progesterone. This leads to estrogen dominance, irregular bleeding, and increased endometrial cancer risk over time.
Often: High Insulin
Insulin stimulates androgen production and lowers SHBG (meaning more free testosterone). This creates a vicious cycle—high insulin drives PCOS, and PCOS worsens insulin resistance.
Treatment: Beyond "Just Take the Pill"

The standard treatment for PCOS is birth control pills. They work—they suppress your hormones and create artificial "periods." But they don't fix anything. They mask the problem while the underlying dysfunction continues.
When you stop the pill, everything comes back. Often worse, because the root cause was never addressed.
A Better Approach
1. Identify Your Type
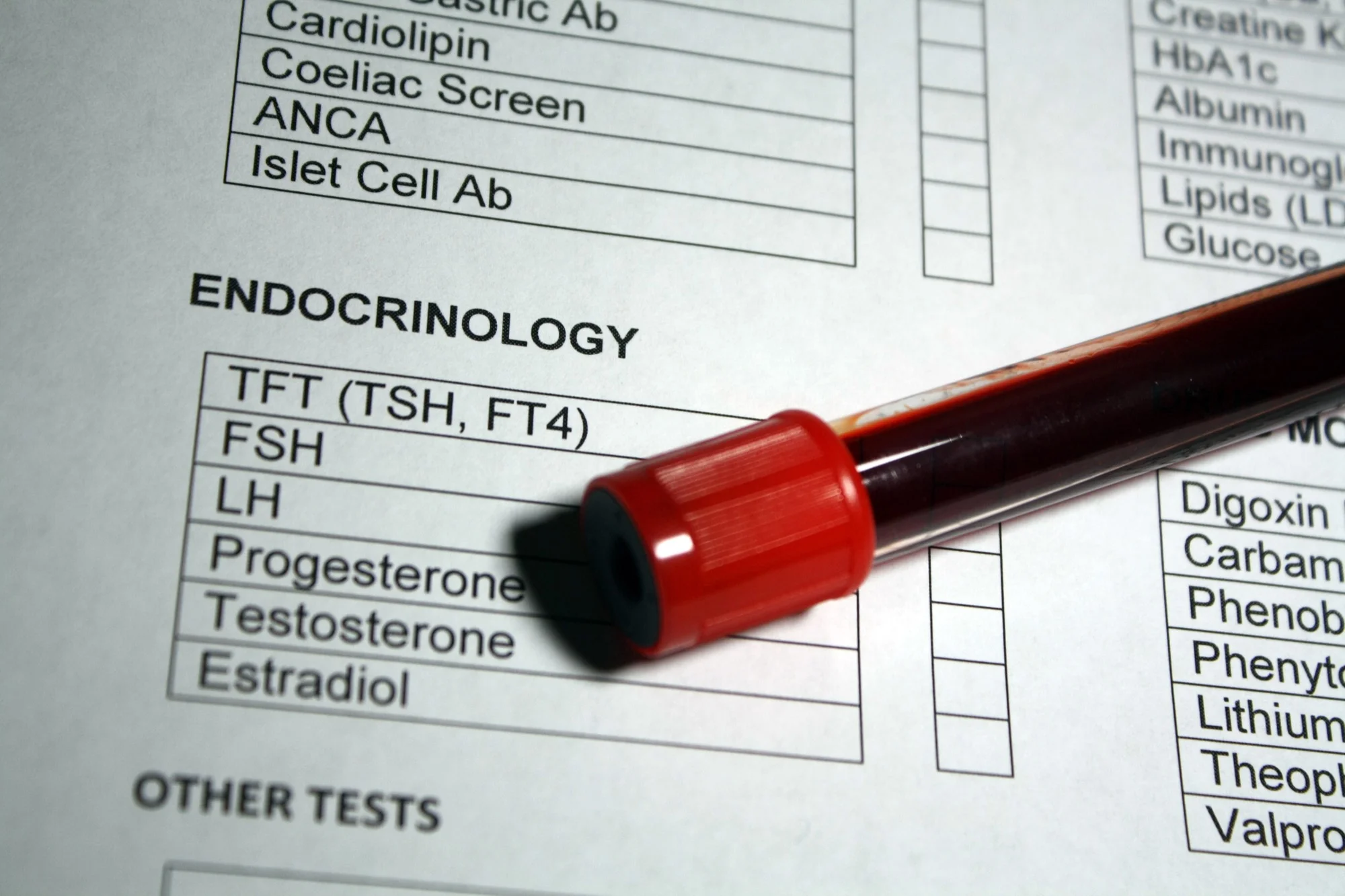
Comprehensive labs including fasting insulin, DHEA-S, testosterone (free and total), SHBG, thyroid panel, and inflammatory markers. Don't guess—test.
2. Address Insulin Resistance (If Present)
Dietary changes (lower glycemic load), strength training, metformin, and/or inositol. Weight loss of even 5-10% can restore ovulation in insulin-resistant PCOS.
3. Support Ovulation
Once the underlying driver is addressed, ovulation often returns. If not, options like letrozole or clomiphene can help. The goal is restoring natural cycling, not suppressing it.
4. Manage Symptoms While Working on Root Cause
Spironolactone for acne/hirsutism, topical treatments, laser hair removal. These don't fix PCOS but improve quality of life while you address the underlying issues.
5. Protect the Uterus
Without regular ovulation, the uterine lining isn't shed properly. If you're not restoring cycles, cyclic progesterone (or yes, sometimes the pill) prevents endometrial hyperplasia.
PCOS and Long-Term Health
PCOS isn't just about irregular periods and acne. It's associated with increased risk of several serious conditions:
Metabolic Risks
- • Type 2 diabetes (4-7x increased risk)
- • Metabolic syndrome
- • Cardiovascular disease
- • Non-alcoholic fatty liver disease
Other Risks
- • Endometrial cancer (2-6x increased)
- • Depression and anxiety
- • Sleep apnea
- • Infertility and pregnancy complications
This is why treating the root cause matters—not just for fertility or cosmetic concerns, but for long-term health.
Labs to Request

If you suspect PCOS or want to understand your type better, these are the key labs:
Hormones
- • LH and FSH (day 2-4 of cycle)
- • Total and free testosterone
- • DHEA-S
- • SHBG
- • Estradiol
- • Progesterone (day 21)
- • AMH (ovarian reserve)
Metabolic & Other
- • Fasting insulin
- • Fasting glucose
- • HbA1c
- • Lipid panel
- • Full thyroid panel (TSH, free T3, T4)
- • hsCRP
- • Prolactin (rule out other causes)
References
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks. Fertil Steril. 2004.
- Teede HJ, et al. International PCOS Network. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod. 2018.
- Azziz R, et al. The Androgen Excess and PCOS Society criteria for the polycystic ovary syndrome. Fertil Steril. 2009.
- Moran LJ, et al. Dietary composition in the treatment of polycystic ovary syndrome: a systematic review. Hum Reprod Update. 2009.
- Legro RS, et al. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2013.
Ready to Find Your Root Cause?
Get comprehensive testing to identify your PCOS type and create a treatment plan that addresses the underlying problem.
Book Your Consultation