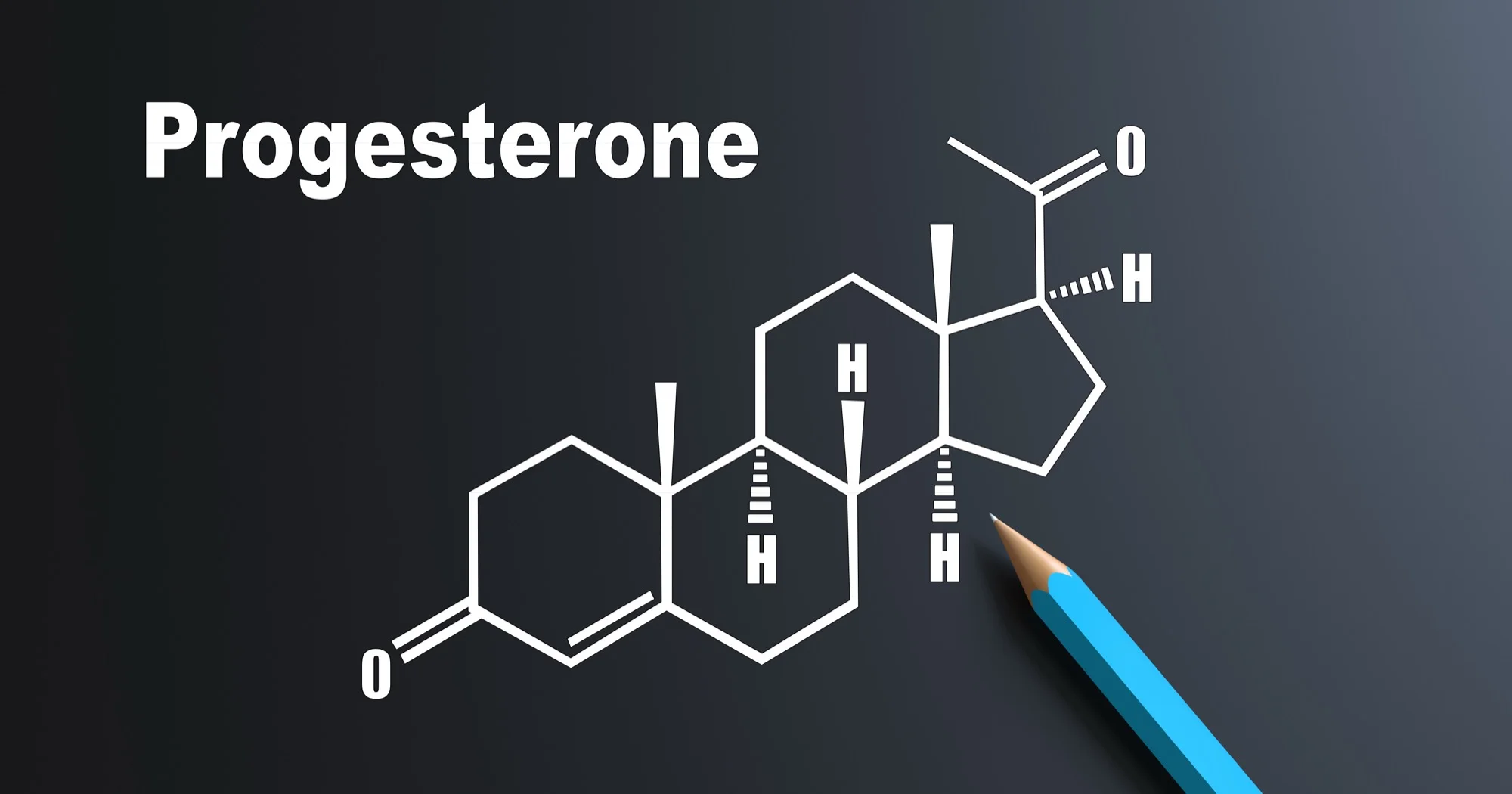
More Than a "Pregnancy Hormone"
When most people think of progesterone, they think of pregnancy and fertility. That's fair—progesterone does prepare the uterine lining for implantation and supports early pregnancy. But reducing it to "the pregnancy hormone" misses the bigger picture.
Progesterone has receptors throughout your brain and body. It affects your nervous system, your sleep architecture, your mood, and your sense of calm. When progesterone drops—whether from anovulatory cycles, perimenopause, or stress—the effects go far beyond fertility.
Understanding progesterone is essential for understanding why you might feel anxious, sleep poorly, or feel "off" even when estrogen levels look fine.
What Progesterone Actually Does
Calms the Nervous System
Progesterone metabolizes into allopregnanolone, a neurosteroid that acts on GABA receptors—the same receptors targeted by anti-anxiety medications and alcohol. This is why progesterone has a natural calming, anti-anxiety effect. When progesterone drops, many women experience increased anxiety, irritability, and a feeling of being "on edge."
Supports Deep Sleep
Through its GABA effects, progesterone promotes deeper, more restorative sleep. Women often notice sleep disturbances in the luteal phase (after ovulation) when progesterone should be high but isn't, and sleep problems are one of the first complaints in perimenopause when progesterone production becomes erratic.
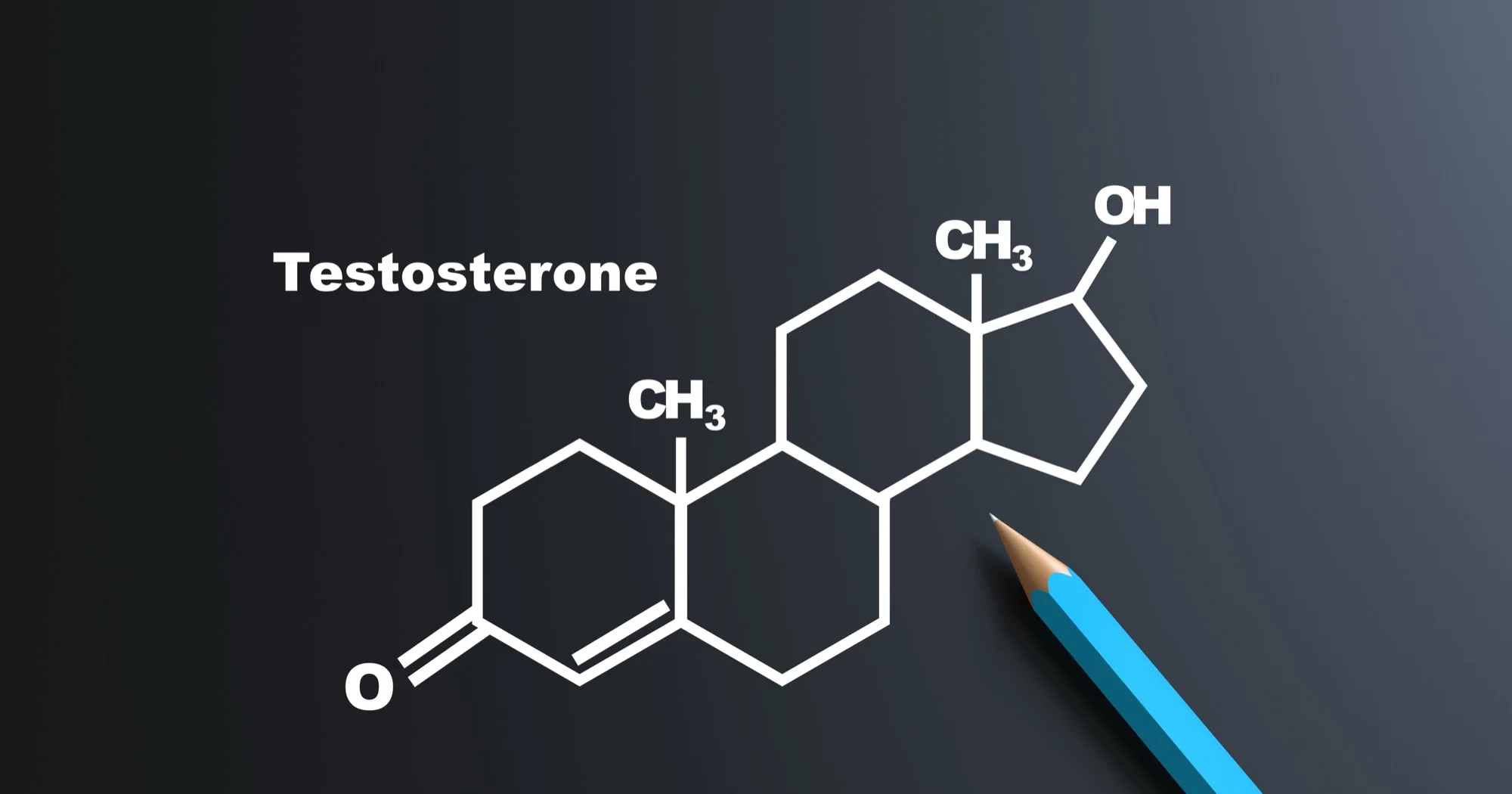
Balances Estrogen
Estrogen and progesterone work in opposition. Estrogen stimulates and builds; progesterone calms and sheds. Without adequate progesterone to balance estrogen, you can develop "estrogen dominance"—not necessarily high estrogen, but estrogen that's unopposed. This leads to heavy periods, breast tenderness, bloating, and mood swings.
Protects the Uterine Lining
Estrogen causes the uterine lining to grow. Progesterone causes it to mature and shed in a controlled way. Without progesterone, the lining can become too thick (hyperplasia), which increases cancer risk over time. This is why women on estrogen therapy always need progesterone if they have a uterus.
Supports Mood Stability
Beyond its anti-anxiety effects, progesterone influences serotonin and other neurotransmitters. Low progesterone is associated with increased depression and mood volatility. Many women notice significant mood changes in the days before their period when progesterone drops sharply.
When Progesterone Drops: The Symptoms
Low progesterone—or a poor progesterone-to-estrogen ratio—can cause a wide range of symptoms that are often attributed to other causes:
Sleep Issues
- • Difficulty falling asleep
- • Waking at 2-4am
- • Light, unrefreshing sleep
- • Vivid dreams or nightmares
Mood & Mental
- • Anxiety without clear cause
- • Irritability, low patience
- • Depression or flat mood
- • Brain fog, poor concentration
Menstrual Changes
- • Heavy or prolonged periods
- • Spotting before period starts
- • Short luteal phase (<10 days)
- • Irregular cycles
Physical Symptoms
- • Breast tenderness
- • Bloating, water retention
- • Headaches (especially premenstrual)
- • Weight gain (especially midsection)
Many women are told these symptoms are "just stress" or "just PMS." While stress absolutely affects hormones, these symptoms often have a clear hormonal driver that can be measured and addressed.
Why Progesterone Declines
Anovulatory Cycles
Progesterone is produced by the corpus luteum—the structure that forms after ovulation. No ovulation = no corpus luteum = no significant progesterone production. Anovulatory cycles are common with PCOS, high stress, under-eating, over-exercising, and in perimenopause.
Perimenopause
Progesterone is the first hormone to decline in perimenopause—often years before estrogen drops. This is why perimenopausal symptoms often start with sleep issues, anxiety, and cycle changes rather than hot flashes. Many women in their late 30s and 40s have declining progesterone while estrogen remains normal or even high.
Chronic Stress
Cortisol (the stress hormone) and progesterone share a precursor: pregnenolone. Under chronic stress, your body prioritizes cortisol production over progesterone—a phenomenon sometimes called "pregnenolone steal." High stress literally diverts resources away from progesterone production.
Luteal Phase Deficiency
Even when ovulation occurs, the corpus luteum may not produce adequate progesterone. This can result from poor follicle development, thyroid issues, or other factors. The result is a short luteal phase (less than 10 days) and low progesterone symptoms despite ovulating.
Testing Progesterone
Timing matters enormously when testing progesterone. In cycling women, progesterone is only elevated in the luteal phase (after ovulation). Testing on day 3 of your cycle will show low progesterone because it's supposed to be low then.
When to Test
For cycling women: Test progesterone 5-7 days after ovulation (approximately day 19-21 of a 28-day cycle, or 7 days before expected period).
For perimenopausal or menopausal women: Timing is less critical as cycles are irregular or absent. Random testing can still provide useful information.
What Levels Mean
Mid-luteal progesterone (day 21):
- • <3 ng/mL: Likely anovulatory
- • 3-10 ng/mL: Ovulation occurred, but may be suboptimal
- • 10-20 ng/mL: Normal, healthy luteal function
- • >20 ng/mL: Robust progesterone production
Note: "Normal" lab ranges are very wide. A level of 5 ng/mL may be flagged as "normal" but still associated with symptoms and fertility issues.
Progesterone Replacement Options
Oral Micronized Progesterone (Prometrium)
Bioidentical progesterone taken by mouth. Has strong sedative/sleep effects due to first-pass liver metabolism (produces more allopregnanolone). Typically taken at bedtime. This is the form with the most evidence for cardiovascular and breast safety when used with estrogen therapy.
Topical/Vaginal Progesterone
Creams, gels, or vaginal suppositories. Bypasses liver metabolism, so less sedation but also less systemic effect. Vaginal application provides good uterine protection. Topical creams have variable absorption and may not provide adequate levels for some purposes.
Progestins (Synthetic)
Synthetic versions like medroxyprogesterone (Provera) are NOT the same as bioidentical progesterone. They protect the uterus but don't provide the neurological benefits and may have different risk profiles. The WHI study used Provera, not bioidentical progesterone—an important distinction.
Important: Progesterone therapy should be individualized based on symptoms, lab values, and whether you still have a uterus. Cycling women may benefit from luteal-phase-only supplementation; post-menopausal women on estrogen need continuous progesterone for uterine protection.
Supporting Progesterone Naturally
While replacement is sometimes necessary, supporting your body's own progesterone production can help—especially for cycling women with luteal phase issues:
Manage Stress
Chronic cortisol elevation competes with progesterone production. Stress management isn't just self-care—it's hormone care.
Eat Enough
Under-eating and over-exercising suppress ovulation. Your body won't prioritize reproduction (and progesterone) if it senses scarcity.
Support Thyroid Function
Hypothyroidism is associated with anovulation and luteal phase defects. Optimal thyroid function supports healthy progesterone production.
Key Nutrients
Vitamin B6, zinc, magnesium, and vitamin C support corpus luteum function and progesterone synthesis. Deficiencies are common.
References
- Prior JC. Progesterone for Symptomatic Perimenopause Treatment. Endocrine Reviews. 2018.
- Schüssler P, et al. Progesterone reduces wakefulness in sleep EEG. Psychoneuroendocrinology. 2008.
- Bäckström T, et al. Allopregnanolone and mood disorders. Progress in Neurobiology. 2014.
- The NAMS 2022 Hormone Therapy Position Statement. Menopause. 2022.
- Fournier A, et al. Breast cancer risk in relation to different types of hormone replacement therapy. Int J Cancer. 2005.
Think Progesterone Might Be the Missing Piece?
Get your hormones tested properly—with the right timing and interpretation.
Book Your Consultation