Rehab & Recovery
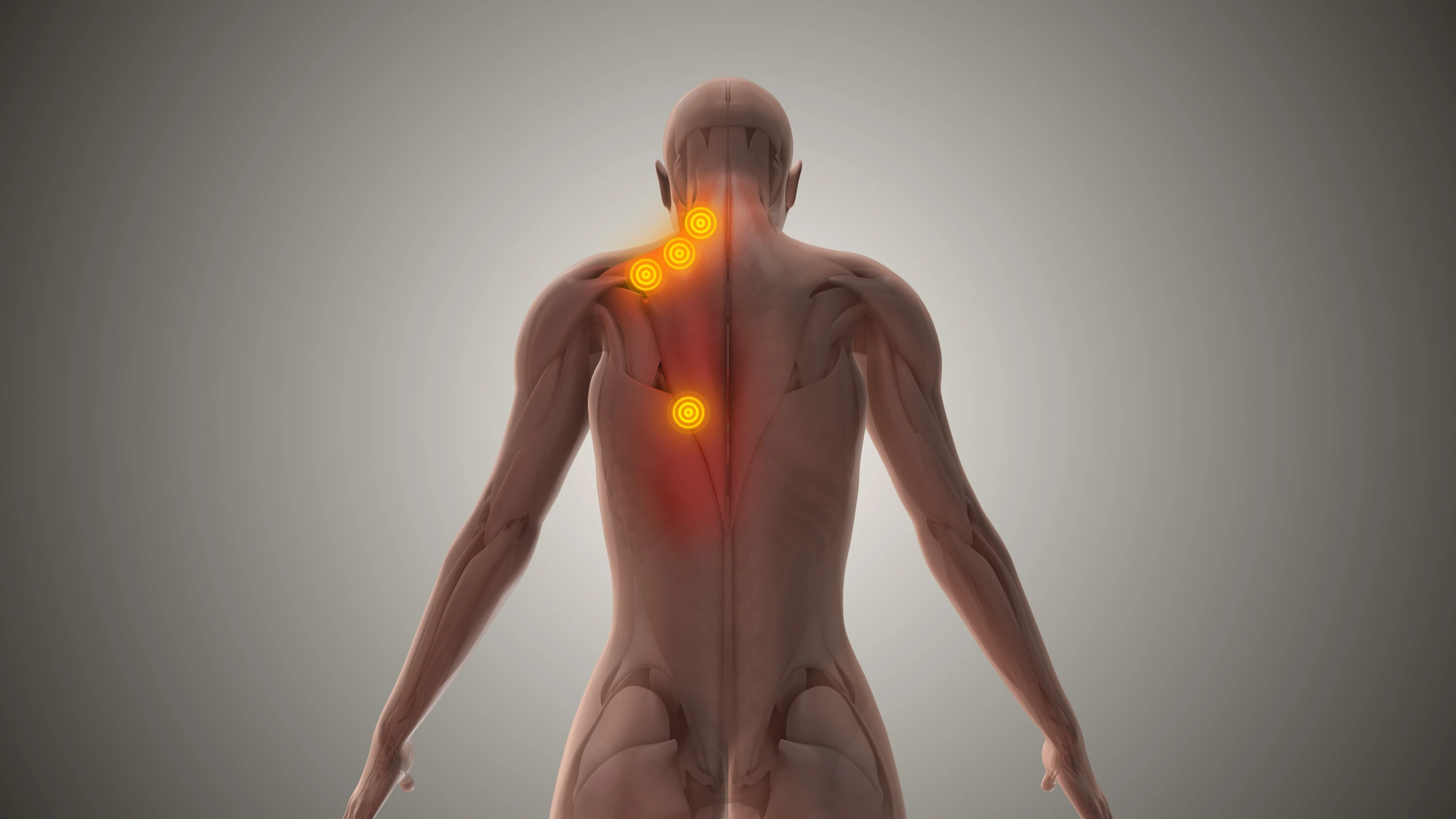
TRIGGER POINT INJECTIONS
What they are, how they mechanically and chemically disrupt chronic muscle knots, and what to expect from the procedure.
WHAT ARE TRIGGER POINT INJECTIONS?
A trigger point injection (TPI) is a medical procedure where a small needle is inserted directly into a myofascial trigger point and a therapeutic solution is injected. The needle itself mechanically disrupts the contracted muscle fibers at the trigger point, while the injected medication provides additional pain relief, reduces local inflammation, and helps the muscle relax.
The procedure is quick, performed in-office, and provides relief that ranges from immediate to within a few days depending on the severity and chronicity of the trigger point. For many patients, it's the intervention that finally breaks the pain cycle that stretching, massage, and over-the-counter medications couldn't resolve.
Trigger point injections have been a staple of pain management and musculoskeletal medicine for decades. They're well-studied, widely used, and effective for a range of conditions rooted in myofascial dysfunction.
Key point: Trigger point injections work through a dual mechanism. The needle physically disrupts the dysfunctional tissue (similar to dry needling), while the injected solution adds a chemical component that enhances pain relief and muscle relaxation. This combination is often more effective than either approach alone.
WHAT ARE TRIGGER POINTS?
A trigger point is a hyperirritable spot within a taut band of skeletal muscle. If you've ever felt a "knot" in your neck, shoulder, or back that's tender to the touch and causes pain to radiate to another area when pressed, you've felt a trigger point.
Trigger points form when muscle fibers become stuck in a contracted state. This isn't a normal muscle contraction you can consciously release. The fibers are locked in a sustained shortening at the microscopic level, creating a palpable nodule within the muscle.
How They Form
Trigger points develop from sustained postures (desk work, phone use), repetitive motions (overhead lifting, typing), acute injury (whiplash, muscle strains), emotional stress (jaw clenching, shoulder guarding), or chronic overload without adequate recovery. Any situation where a muscle is held in contraction or repeatedly overworked beyond its recovery capacity can create trigger points.
The Energy Crisis Theory (Simons & Travell)
The most widely accepted explanation comes from Drs. Janet Travell and David Simons, who pioneered the field of myofascial pain. Their "integrated trigger point hypothesis" describes an energy crisis at the motor endplate (the junction where nerve meets muscle). Excessive acetylcholine release causes sustained muscle fiber contraction. This compression restricts local blood flow, creating an oxygen and energy deficit. The energy deficit prevents the muscle from releasing the contraction, and metabolic waste products accumulate, sensitizing local pain receptors. The result is a self-perpetuating cycle: contraction leads to ischemia, which leads to energy crisis, which prevents the muscle from relaxing.
Local Pain vs. Referred Pain
Trigger points cause two types of pain. Local pain is tenderness and aching right at the trigger point itself. Referred pain is the more distinctive feature: pressing on a trigger point in the upper trapezius can cause pain to radiate up into the head (a common cause of tension headaches). A trigger point in the infraspinatus can send pain down the arm. These referred pain patterns are consistent and well-mapped, which is what makes trigger points identifiable and treatable.
Restricted Range of Motion
Because the affected muscle fibers are locked in contraction, the muscle can't fully lengthen. This creates stiffness, limited range of motion, and compensatory movement patterns. Over time, surrounding muscles begin to overwork to compensate, often developing their own trigger points. A single untreated trigger point can cascade into a regional pain pattern.
HOW THE INJECTION WORKS
Trigger point injections work through two complementary mechanisms: mechanical disruption from the needle and chemical effect from the injected solution. Understanding both explains why the procedure is more effective than simply taking a pain reliever or getting a massage.
Mechanical Disruption
The needle physically penetrates the trigger point and disrupts the dysfunctional motor endplate. This is similar to what happens in dry needling. The needle breaks up the contracted sarcomeres (the smallest contractile units of muscle fiber), interrupts the abnormal acetylcholine feedback loop, and creates a local microtrauma that stimulates a healing response. The "local twitch response" that often occurs during the procedure is a brief, involuntary contraction of the muscle fiber, which is a reliable sign that the needle has hit the trigger point and disrupted it.
Chemical Effect
The injected solution adds a second layer of therapeutic effect. Lidocaine (the most common injectate) provides immediate local anesthesia, blocking pain signals from the treated area and interrupting the pain-spasm-pain cycle. It also has direct muscle-relaxing properties. When a corticosteroid is added, it reduces local inflammation and can provide longer-lasting relief for trigger points with a significant inflammatory component. Even saline has been shown to be beneficial by diluting the concentrated metabolic waste products trapped in the trigger point and mechanically separating contracted fibers.
Why the combination matters: Research consistently shows that the combination of mechanical needling plus an injected solution produces better outcomes than either alone. The needle disrupts the structural problem while the medication addresses the chemical environment. This is why trigger point injections often succeed where other treatments have plateaued.
WHAT'S INJECTED
The solution injected into a trigger point varies depending on the clinical scenario. There isn't a single "best" option for every patient. A good provider matches the injectate to the specific presentation.
Lidocaine (Most Common)
Lidocaine is a local anesthetic and the most widely used injectate for trigger point injections. It provides immediate pain relief by blocking sodium channels in nerve fibers, preventing pain signal transmission. It also has direct muscle-relaxant properties. Lidocaine is preferred for most trigger point injections because it provides fast-acting relief, has a well-established safety profile, is unlikely to cause tissue irritation, and its anesthetic effect helps break the pain-spasm cycle immediately. Concentrations used are typically 0.5% to 1%, which is lower than what's used for procedures like dental work.
Lidocaine + Corticosteroid
When there's a significant inflammatory component, such as a trigger point associated with a chronic overuse injury or an acute flare-up with visible swelling or heat, a corticosteroid (such as triamcinolone or dexamethasone) may be combined with the lidocaine. The steroid provides potent anti-inflammatory effects that can extend the duration of relief. This combination is appropriate for chronic trigger points that haven't responded to lidocaine alone, trigger points near inflamed tendons or bursae, and patients with underlying inflammatory conditions. Steroid use is typically limited to avoid the tissue-thinning effects of repeated corticosteroid injections at the same site.
Saline (Normal Saline)
Isotonic saline (0.9% sodium chloride) is sometimes used as the injectate, particularly for patients who are sensitive or allergic to local anesthetics. Saline works by mechanically separating contracted muscle fibers, diluting the concentrated metabolic waste products and inflammatory mediators trapped in the trigger point, and providing a volume effect that stretches the local tissue. Studies have shown that saline injections into trigger points can be effective, reinforcing the importance of the mechanical needling component of the procedure.
Dry Needling (No Injectate)
Technically, dry needling uses no injected solution at all. The needle alone provides the mechanical disruption. While not a "trigger point injection" in the traditional sense, it's part of the same treatment spectrum. Dry needling is often performed by physical therapists and chiropractors and relies entirely on the mechanical disruption mechanism. Some patients prefer it because no medication is involved. We cover the comparison between TPIs and dry needling in detail below.
HOW THE PROCEDURE IS PERFORMED
The procedure is straightforward, performed in-office, and typically completed in 10 to 20 minutes.
Identification & Palpation
The provider palpates the affected muscle to locate the trigger point. This involves running their fingers across the muscle fibers to find the taut band, then isolating the nodule within it. The trigger point is pinched or pressed between two fingers (or between a finger and the underlying bone) to stabilize it for needle insertion. The patient confirms the location by recognizing their familiar pain pattern when the point is pressed.
Skin Preparation
The skin over the trigger point is cleaned with an antiseptic solution (typically alcohol or chlorhexidine) to minimize infection risk. Some providers apply a topical numbing spray (ethyl chloride or vapocoolant) to reduce the initial needle stick sensation, though this is optional since the discomfort from the insertion is brief.
Needle Insertion & Injection
A small-gauge needle (typically 22 to 25 gauge) is inserted directly into the trigger point. The provider advances the needle into the taut band while injecting the solution. A key technique is "fanning" or "peppering," where the needle is partially withdrawn and redirected multiple times through the trigger point in slightly different directions. This ensures the entire trigger point is mechanically disrupted and the solution is distributed throughout the affected area.
Local Twitch Response
When the needle penetrates the trigger point, the patient often experiences a brief, involuntary muscle twitch. This local twitch response (LTR) is a good sign. Research by Hong and Simons showed that eliciting a local twitch response during needling is associated with significantly better treatment outcomes. It confirms the needle is in the right spot and that the dysfunctional motor endplate is being disrupted. The twitch lasts a fraction of a second and, while it can be startling, is not painful.
Post-Injection Care
After the needle is removed, the provider applies direct pressure to the injection site for 1 to 2 minutes to prevent bleeding and help distribute the solution. The patient is then guided through gentle stretching of the treated muscle. This post-injection stretch is important because it helps restore the muscle to its full resting length while the trigger point is deactivated and the area is anesthetized.
WHAT CONDITIONS DO TRIGGER POINT INJECTIONS TREAT?
Trigger point injections are effective for any condition where myofascial trigger points are a primary or contributing cause of pain. That covers a wide range of musculoskeletal complaints.
Chronic Neck & Shoulder Tension
The upper trapezius and levator scapulae are among the most common trigger point locations. Desk work, phone use, and stress create sustained contraction in these muscles. Trigger points here cause neck stiffness, shoulder pain, and frequently refer pain into the head.
Tension Headaches
Many tension-type headaches are caused or exacerbated by trigger points in the upper trapezius, sternocleidomastoid, suboccipital, and temporalis muscles. These trigger points refer pain into the head in patterns that mimic tension headaches. Deactivating the trigger points can reduce headache frequency and intensity.
Low Back Pain
Trigger points in the quadratus lumborum, paraspinal muscles, gluteus medius, and piriformis are frequent contributors to chronic low back pain. These trigger points can mimic disc-related pain, sciatica, or sacroiliac joint dysfunction. Identifying and treating the myofascial component often provides relief that imaging-guided interventions miss.
Myofascial Pain Syndrome
Myofascial pain syndrome (MPS) is a chronic pain condition defined by the presence of multiple active trigger points. It's one of the most underdiagnosed causes of chronic musculoskeletal pain. Trigger point injections are a primary treatment modality for MPS, often combined with physical therapy and postural correction.
Fibromyalgia
While fibromyalgia involves widespread pain and central sensitization, many fibromyalgia patients have concurrent myofascial trigger points that amplify their pain. Treating these peripheral pain generators with trigger point injections can reduce overall pain burden and improve quality of life as part of a comprehensive management plan.
TMJ-Related Muscle Pain
The masseter, temporalis, and medial pterygoid muscles can develop trigger points from jaw clenching, teeth grinding (bruxism), or TMJ dysfunction. These trigger points cause jaw pain, limited mouth opening, and can refer pain to the teeth, ear, and temple. Trigger point injections to the masticatory muscles can provide significant relief.
Chronic Muscle Spasms
Recurrent or persistent muscle spasms that don't respond to stretching, heat, or oral muscle relaxants are often driven by underlying trigger points. The injection breaks the spasm cycle at its source rather than masking it systemically with medication.
Post-Injury Muscle Guarding
After an injury (car accident, sports injury, fall), surrounding muscles often "guard" by tightening protectively. This guarding can persist long after the original injury heals, creating chronic trigger points that become a secondary pain source. Trigger point injections can release this residual muscle guarding and accelerate return to normal function.
WHAT TO EXPECT
Knowing what the experience is actually like helps you prepare and set realistic expectations.
During the Procedure
You'll feel a mild sting when the needle enters the skin, similar to a blood draw. As the needle reaches the trigger point, you may feel a brief deep ache or cramping sensation, followed by the local twitch response (a quick involuntary muscle jump). This is the moment the trigger point is disrupted. The entire injection takes about 15 to 30 seconds per trigger point. Most patients describe the discomfort as brief and very tolerable, especially compared to the chronic pain they've been dealing with.
Immediately After
Many patients feel immediate relief as the lidocaine takes effect and the trigger point is deactivated. The muscle often feels noticeably looser and range of motion improves right away. Some patients describe a "release" sensation, as if the muscle has finally let go of tension it's been holding for weeks or months.
24 to 48 Hours Post-Injection
As the lidocaine wears off (usually within a few hours), you may experience soreness at the injection site. This is normal and similar to the feeling after a deep tissue massage or an intense workout. Mild bruising can occur. Applying ice and gentle stretching during this period helps. Avoid intense exercise or heavy loading of the treated muscle for 24 to 48 hours.
Full Effect
The full benefit of the injection typically develops over the first 3 to 7 days as the local inflammation resolves and the muscle adapts to its restored resting length. Some patients experience complete resolution after a single treatment. Chronic or longstanding trigger points may require a series of sessions spaced 2 to 4 weeks apart, often combined with corrective exercises and postural modifications to prevent recurrence.
Long-Term Outlook
Trigger point injections are most effective when combined with an active approach: corrective stretching, strengthening weak muscles, ergonomic adjustments, and addressing the root cause that created the trigger points in the first place. The injection breaks the pain cycle and restores function. The follow-up rehab keeps it from coming back.
TRIGGER POINT INJECTIONS VS. DRY NEEDLING
Both trigger point injections and dry needling target the same structures: myofascial trigger points. They share the same mechanical disruption mechanism. The key difference is whether a solution is injected.
Trigger Point Injections
- Needle insertion plus an injected solution (lidocaine, corticosteroid, or saline)
- Performed by physicians, nurse practitioners, and physician assistants
- Dual mechanism: mechanical disruption plus chemical effect
- Often provides faster initial relief due to the anesthetic component
- Better suited for patients with severe pain who need immediate relief
- Can include anti-inflammatory medication for inflammatory presentations
- Typically uses a larger gauge needle (22-25 gauge)
Dry Needling
- Needle insertion without any injected solution
- Performed by physical therapists, chiropractors, and other trained providers
- Relies solely on mechanical disruption of the trigger point
- May require more needle manipulation to achieve full effect
- Preferred by patients who want to avoid any medication
- Often uses thinner acupuncture-style needles (filiform needles)
- Can be integrated into a physical therapy treatment session
The bottom line: These are complementary approaches, not competing ones. Some patients respond better to one than the other. In many cases, using both within a treatment plan produces the best results. A trigger point injection can break through a severe, longstanding trigger point, and follow-up dry needling during physical therapy can maintain the result and address secondary trigger points. The best approach depends on the severity of the trigger point, your pain tolerance, your treatment goals, and your provider's clinical judgment.
COMMON QUESTIONS
How long does a trigger point injection take?
The injection itself takes about 15 to 30 seconds per trigger point. A full session treating multiple trigger points typically takes 10 to 20 minutes, including preparation. Most patients are in and out of the office within 30 minutes.
How many sessions will I need?
It depends on the severity and chronicity of your trigger points. Some patients experience complete relief after a single session. Chronic or recurring trigger points may require a series of 3 to 6 sessions spaced 2 to 4 weeks apart. Your provider will assess your response after each treatment and adjust the plan accordingly. The goal is always resolution, not indefinite treatment.
What are the side effects?
The most common side effect is temporary soreness at the injection site, similar to a deep bruise, lasting 24 to 48 hours. Minor bruising can occur. Serious side effects are rare but can include infection at the injection site (minimized by proper skin preparation), allergic reaction to the anesthetic (uncommon with lidocaine), or temporary numbness if a nerve is near the injection site. When performed by a trained provider using proper technique, trigger point injections are very safe.
Does insurance cover trigger point injections?
Many insurance plans cover trigger point injections when they are medically necessary and performed by a licensed provider. Coverage varies by plan and diagnosis. Trigger point injections are billed under CPT codes 20552 (1 to 2 muscles) or 20553 (3 or more muscles). Check with your insurance provider for specific coverage details, or ask our office to verify benefits before your appointment.
Can I exercise after a trigger point injection?
Light activity and gentle stretching are encouraged after the injection. Avoid intense exercise or heavy loading of the treated muscle group for 24 to 48 hours to allow the tissue to recover and reduce the risk of rebound soreness. After that window, you can return to normal activity. Your provider may also recommend specific stretches or corrective exercises to maximize the benefit of the injection and prevent the trigger point from returning.
References
- 1. Travell JG, Simons DG. Myofascial Pain and Dysfunction: The Trigger Point Manual. Vol 1 & 2. Williams & Wilkins; 1983, 1992.
- 2. Simons DG. "Review of enigmatic MTrPs as a common cause of enigmatic musculoskeletal pain and dysfunction." J Electromyogr Kinesiol. 2004;14(1):95-107.
- 3. Hong CZ. "Lidocaine injection versus dry needling to myofascial trigger point: the importance of the local twitch response." Am J Phys Med Rehabil. 1994;73(4):256-263.
- 4. Alvarez DJ, Rockwell PG. "Trigger points: diagnosis and management." Am Fam Physician. 2002;65(4):653-660.
- 5. Scott NA, Guo B, Barton PM, Gerwin RD. "Trigger point injections for chronic non-malignant musculoskeletal pain: a systematic review." Pain Med. 2009;10(1):54-69.
- 6. Borg-Stein J, Simons DG. "Focused review: myofascial pain." Arch Phys Med Rehabil. 2002;83(3 Suppl 1):S40-S47.
- 7. Cummings TM, White AR. "Needling therapies in the management of myofascial trigger point pain: a systematic review." Arch Phys Med Rehabil. 2001;82(7):986-992.
- 8. Gerwin RD. "Classification, epidemiology, and natural history of myofascial pain syndrome." Curr Pain Headache Rep. 2001;5(5):412-420.
- 9. Shah JP, Thaker N, Heimur J, Aredo JV, Sikdar S, Gerber L. "Myofascial Trigger Points Then and Now: A Historical and Scientific Perspective." PM R. 2015;7(7):746-761.
- 10. Rickards LD. "The effectiveness of non-invasive treatments for active myofascial trigger point pain: a systematic review of the literature." Int J Osteopath Med. 2006;9(4):120-136.
STRUGGLING WITH CHRONIC MUSCLE PAIN?
Trigger point injections can break the cycle of chronic muscle tension and referred pain. We'll identify the source, treat it directly, and build a plan to keep it from coming back.
Book Consultation