Diagnostics
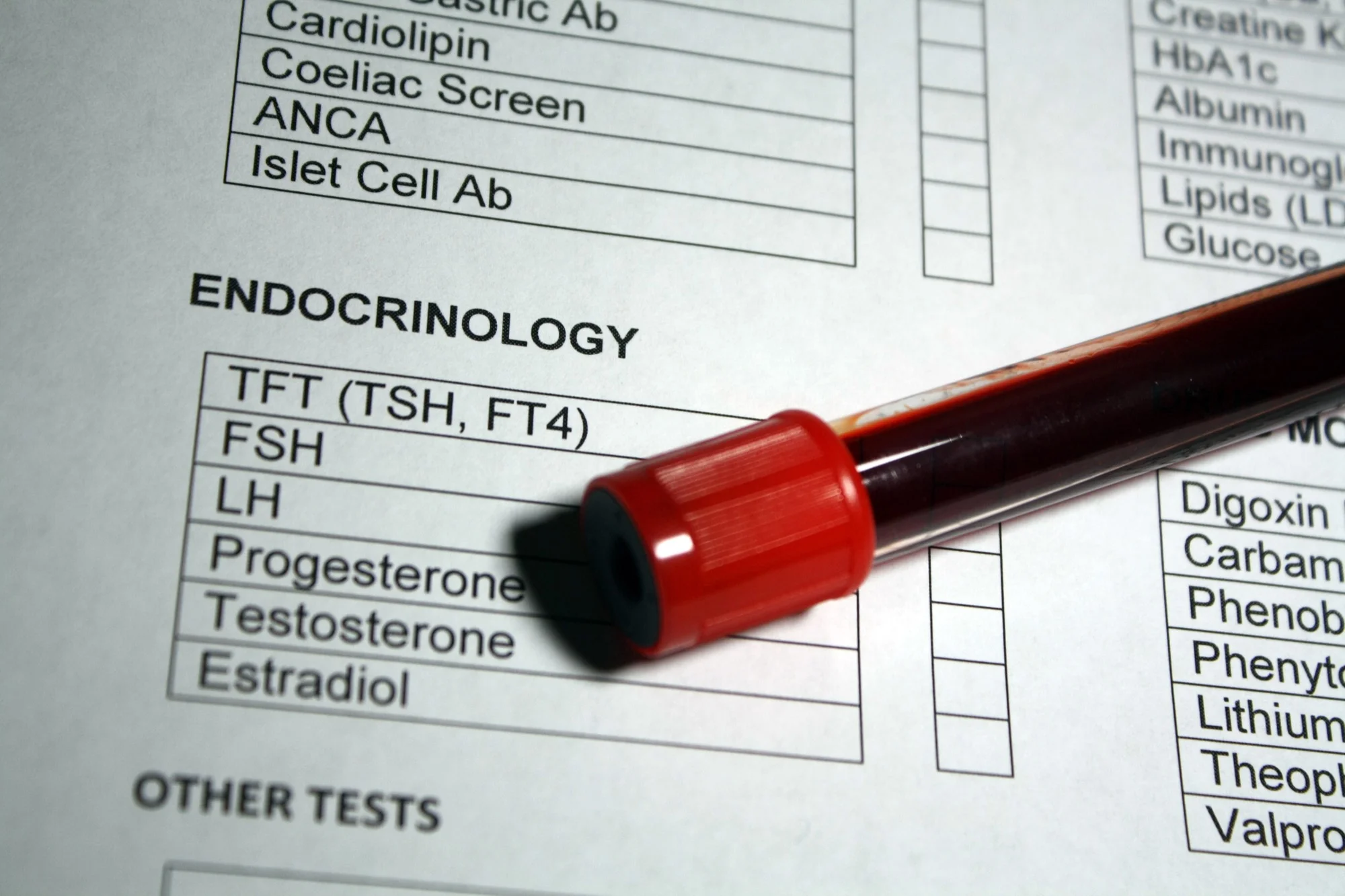
WHAT LABS SHOULD YOU ACTUALLY BE TESTING?
Your annual physical checks a handful of markers and calls it a day. That panel was designed to catch disease, not optimize health. Here's what a real lab panel looks like.
The Problem With Standard Blood Panels
- 1. Most annual panels test only 12-15 markers
- 2. Critical markers like fasting insulin, ApoB, and Free T3 are almost never included
- 3. "Normal" reference ranges are based on sick and sedentary populations
- 4. Hormones are usually ignored entirely until symptoms are severe
- 5. Nutrient deficiencies go undetected for years
- 6. Cardiovascular risk is assessed with outdated lipid panels
A comprehensive panel tests 50-80+ markers and reveals what standard blood work misses. It's the difference between asking "Am I sick?" and asking "How do I perform at my best?"
WHAT A STANDARD PANEL MISSES
Here's a side-by-side look at what a typical annual physical checks versus what a comprehensive optimization panel includes. The gap is significant.
Typical Annual Physical Panel
- • Complete Blood Count (CBC)
- • Basic Metabolic Panel (glucose, electrolytes)
- • Standard Lipid Panel (Total Cholesterol, LDL, HDL, Triglycerides)
- • TSH only (thyroid screening)
- • Maybe HbA1c if you're high risk
- • Maybe PSA if you ask
12-15 markers. Designed to screen for disease.
Comprehensive Optimization Panel
- • Everything above, plus...
- • Fasting Insulin, HOMA-IR (metabolic health)
- • Full Thyroid: Free T3, Free T4, T3 Uptake, TPO/TG Antibodies
- • Total & Free Testosterone, Estradiol, DHEA-S, SHBG
- • ApoB, Lp(a), LDL-P, hs-CRP, Homocysteine
- • Vitamin D, RBC Magnesium, Iron Panel, B12, Folate, Zinc
- • Cortisol, Prolactin, IGF-1, Progesterone
50-80+ markers. Designed to optimize function.
The standard panel tells you whether you're diagnosably sick right now. It does not tell you whether you're heading toward disease, whether your hormones are tanking, whether you're insulin resistant, or whether you have a cardiovascular risk that a basic lipid panel completely misses. That's not a feature. It's a limitation.
THE COMPLETE PANEL BREAKDOWN
Here's exactly what we test at Moonshot Medical in Park Ridge, organized by category. Each marker has a purpose.
Hormones
Hormones are the signaling system that governs energy, body composition, mood, cognition, and sexual function. Most doctors check TSH and nothing else. That's like checking the oil light on your dashboard and ignoring the engine.
- Total Testosterone - Overall production
- Free Testosterone - What's bioavailable to tissues
- Estradiol (E2) - Estrogen balance; affects mood, joints, cardiovascular health
- DHEA-S - Adrenal hormone; precursor to testosterone and estrogen
- Progesterone - Often overlooked in men; affects sleep, anxiety, neuroprotection
- TSH - Thyroid-stimulating hormone (screening only)
- Free T3 - Active thyroid hormone; the one that matters most
- Free T4 - Storage form of thyroid hormone
- T3 Uptake - Binding capacity indicator
- TPO & TG Antibodies - Autoimmune thyroid markers
Why it matters: A TSH of 3.5 is "normal" but if Free T3 is low and TPO antibodies are elevated, you have early Hashimoto's thyroiditis that won't show up on a standard panel for years. By then, damage is done.
Metabolic Health
Metabolic dysfunction is the root of most chronic disease. The standard panel checks fasting glucose and maybe HbA1c. That catches diabetes after it's already developed. These markers catch the trajectory years earlier.
- Fasting Insulin - The earliest marker of metabolic dysfunction
- HbA1c - 3-month average blood sugar
- HOMA-IR - Insulin resistance score (calculated from glucose + insulin)
- Comprehensive Metabolic Panel - Kidney, liver, electrolytes
Why it matters: Your fasting glucose can be 95 mg/dL ("normal") while your fasting insulin is 18 mIU/L (high). That means your pancreas is working overtime to keep glucose down. You're insulin resistant, and without fasting insulin on the panel, nobody would know.
Cardiovascular Risk
Standard lipid panels give you total cholesterol, LDL, HDL, and triglycerides. That's a start, but it misses the markers most predictive of heart attack and stroke. Half of all cardiac events occur in people with "normal" cholesterol.
- ApoB - Best single marker for atherogenic risk; counts all damaging particles
- Lp(a) - Genetic risk factor; doesn't change with lifestyle; test once
- LDL-P (Particle Number) - Number of LDL particles; more predictive than LDL-C
- hs-CRP - High-sensitivity C-reactive protein; systemic inflammation
- Homocysteine - Vascular inflammation and methylation marker
- Lp-PLA2 - Arterial inflammation specific to vascular walls
Why it matters: You can have an LDL-C of 110 mg/dL ("normal") and an ApoB of 130 mg/dL (high risk). Your standard panel says you're fine. An advanced cardiovascular panel says you need intervention now.
Nutrient Status
Nutrient deficiencies are wildly common and rarely tested. They affect everything from immune function to energy to hormone production. Supplementing blindly without testing is guessing. Testing gives you targeted intervention.
- Vitamin D (25-OH) - Immune, bone, mood, hormone support; most people are deficient
- RBC Magnesium - Intracellular magnesium; serum magnesium is unreliable
- Iron Panel + Ferritin - Iron stores; too low = fatigue; too high = organ damage
- Vitamin B12 - Energy, nerve function, red blood cell production
- Folate - Methylation, DNA repair, red blood cell health
- Zinc - Immune function, testosterone production, wound healing
Why it matters: Over 40% of Americans are Vitamin D insufficient. RBC Magnesium is low in a majority of people tested at our Park Ridge clinic. These deficiencies cause fatigue, poor sleep, weak immune response, and impaired hormone production. They're also cheap and easy to fix once identified.
Blood Health
- CBC with Differential - Red/white blood cells, platelets, immune cell breakdown
- PSA (Men) - Prostate screening; baseline matters
- Liver Enzymes (AST/ALT/GGT) - Liver function and metabolic stress
Additional Markers
- Cortisol - Stress hormone; affects metabolism, sleep, immune function
- SHBG - Binds testosterone; determines how much is bioavailable
- Prolactin - Elevated levels suppress testosterone and libido
- IGF-1 - Growth hormone proxy; muscle recovery, tissue repair, aging
WHY "NORMAL" RANGES ARE MISLEADING
When your doctor says your labs are "normal," understand what that actually means and why it might not mean what you think.
Lab reference ranges are calculated from the general population. They represent the middle 95% of results from everyone who walks into that lab. That population includes people who are overweight, sedentary, chronically stressed, sleep-deprived, and on multiple medications. When you fall within "normal," you fall within the range of that group. That's a low bar.
Normal vs. Optimal: Real Examples
Vitamin D
Lab Normal: 30-100 ng/mL
Optimal: 50-80 ng/mL
TSH
Lab Normal: 0.5-4.5 mIU/L
Optimal: 1.0-2.0 mIU/L
Fasting Insulin
Lab Normal: 2.6-24.9 mIU/L
Optimal: 3-8 mIU/L
Total Testosterone (Men)
Lab Normal: 264-916 ng/dL
Optimal: 500-900 ng/dL
Ferritin
Lab Normal: 12-300 ng/mL (men)
Optimal: 50-150 ng/mL
hs-CRP
Lab Normal: <3.0 mg/L
Optimal: <1.0 mg/L
This is the gap between optimal and normal. A fasting insulin of 22 is technically normal. Clinically, it signals insulin resistance and a trajectory toward type 2 diabetes. A TSH of 4.0 is normal. But if you're fatigued, cold, constipated, and gaining weight, that TSH might be your answer. The reference range just told you to ignore it.
Optimal ranges come from research on healthy, active populations and from clinical experience with patients who feel and perform their best. They're narrower, and they're more useful.
HOW OFTEN TO TEST
Baseline
Everyone needs a comprehensive baseline. This is your starting point. You can't track progress or identify decline without it. Ideally done before starting any interventions, supplements, or lifestyle changes. Think of it as your health audit.
6-8 Weeks After Intervention
Started hormone therapy? New supplement protocol? Changed your diet significantly? Retest at 6-8 weeks. This shows whether the intervention is working, whether doses need adjustment, and whether there are any unintended effects. Skipping this step is flying blind.
Quarterly (First Year)
During the first year of active optimization, quarterly testing helps dial in protocols. Hormones, insulin sensitivity, inflammatory markers, and nutrient levels can shift meaningfully over 3-month windows. This is where precision matters most.
Semi-Annual or Annual (Maintenance)
Once your numbers are stable and you're feeling good, testing every 6-12 months is sufficient. This catches gradual shifts before they become problems and confirms your protocols are still effective. Adjust the schedule if new symptoms arise or major life changes occur (stress, illness, medication changes).
HOW TO PREPARE FOR ACCURATE RESULTS
Bad preparation means bad data. These details matter. A poorly timed blood draw can make your results look dramatically different from reality.
Fasting
Fast for 10-12 hours before your draw. Water is fine and encouraged (dehydration can affect results). Black coffee is generally acceptable but can slightly affect cortisol. No food, no supplements, no caloric beverages.
Time of Day
Test in the morning, ideally between 7-10 AM. Testosterone peaks in the morning and drops throughout the day. Cortisol follows a diurnal pattern. Testing at 3 PM gives you a fundamentally different picture than 8 AM.
Exercise
Avoid intense exercise for 24 hours before your draw. Heavy training can temporarily spike liver enzymes (AST, ALT), inflammatory markers (CRP), and cortisol, which could be misinterpreted as a problem when it's just recovery.
Medications & Supplements
Ask your provider whether to take medications before or after the draw. Biotin supplements can interfere with thyroid and hormone assays. If you're on TRT, timing relative to your injection matters for accurate trough or peak measurements.
Hydration
Drink plenty of water the evening before and morning of your draw. Dehydration concentrates your blood, which can falsely elevate hemoglobin, hematocrit, and some protein markers. It also makes the draw easier on the phlebotomist.
Consistency
For follow-up labs, replicate conditions. Same time of day, same fasting window, same timing relative to medications. This makes your results comparable across draws so you can identify real trends rather than noise.
WHAT TO DO WITH YOUR RESULTS
Data without interpretation is just numbers on a page. Here's how to actually use your lab results to make better decisions about your health.
Get Interpretation, Not Just Data
A patient portal that shows you green/yellow/red flags is not interpretation. You need someone who understands how markers interact. Low Free T3 with high Reverse T3 tells a different story than low Free T3 alone. Context matters.
Look for Patterns, Not Isolated Numbers
Individual markers rarely tell the full story. High fasting insulin + high triglycerides + low HDL = metabolic syndrome pattern. Elevated SHBG + low Free T + normal Total T = a binding problem, not a production problem. Pattern recognition is where the real insight lives.
Track Trends Over Time
A single lab draw is a snapshot. Multiple draws reveal trajectory. A Vitamin D of 35 ng/mL heading up after supplementation is different from 35 heading down. A slowly rising fasting insulin over 2 years is an early warning. Trends are more valuable than any single number.
At Moonshot Medical, every comprehensive panel comes with a provider consultation. We walk through every result, explain the patterns, compare to your previous draws, and build an action plan. The lab work is only useful if someone helps you understand what it means and what to do about it.
WHAT COMPREHENSIVE TESTING ACTUALLY COSTS
Thorough blood work sounds expensive until you compare it to the alternatives. Here's the real math.
Standard Annual Physical
$50-150
12-15 markers. Basic screening. Misses most of what matters for optimization.
Comprehensive Optimization Panel
$300-800
50-80+ markers. Full picture. Hormones, metabolic, cardiovascular, nutrients, inflammation.
Same Tests A La Carte (Quest/LabCorp)
$2,000+
Same markers ordered individually without a provider. No interpretation included.
The real cost equation: A comprehensive panel at $300-800 is not a premium add-on. It's the standard of care if the goal is actually understanding your health. The standard annual physical was designed for disease screening in the 1960s. It was never designed for optimization. At Moonshot Medical in Park Ridge, we price our panels to make thorough testing accessible to anyone in the Chicago suburbs who wants real answers, not just a clean bill of health that misses everything below the surface.
COMMON QUESTIONS
What blood tests should I ask my doctor to order?
Beyond the standard CBC and metabolic panel, ask for: fasting insulin (not just glucose), HbA1c, a complete thyroid panel (TSH, Free T3, Free T4, TPO antibodies), Total and Free Testosterone, Estradiol, DHEA-S, Vitamin D (25-OH), RBC Magnesium, a full iron panel with ferritin, ApoB, Lp(a), hs-CRP, homocysteine, and SHBG. Most doctors will only order a fraction of these unless you specifically request them.
Why does my doctor say my labs are "normal" when I still feel terrible?
Standard reference ranges are built from the general population, including people who are overweight, sedentary, stressed, and on medications. "Normal" means you fall within the range of average Americans, not that you're optimized. For example, a Vitamin D level of 31 ng/mL is technically normal but far below the 50-80 ng/mL range associated with optimal immune and metabolic function. There's a significant difference between "not diagnosably sick" and "actually healthy."
How often should I get comprehensive blood work done?
Start with a comprehensive baseline. If you begin any intervention (hormone therapy, supplementation, dietary changes), retest at 6-8 weeks. During the first year of optimization, quarterly testing helps dial in your protocol. After that, semi-annual or annual testing is sufficient for most people, unless something changes or new symptoms arise.
Do I need to fast before blood work?
Yes, for the most accurate results. Fast for 10-12 hours before your draw (water is fine and encouraged). Test in the morning, ideally between 7-10 AM, especially if hormones are being measured since testosterone and cortisol peak in the morning. Avoid intense exercise the day before. If you take supplements or medications, ask your provider whether to take them before or after the draw.
How much does comprehensive blood work cost?
A standard annual physical panel runs $50-150 but misses most advanced markers. A comprehensive optimization panel typically costs $300-800 depending on the markers included. If you tried to order the same tests a la carte through Quest or LabCorp without a provider, you could easily pay $2,000 or more. At Moonshot Medical in Park Ridge, IL, our comprehensive panels are priced to make thorough testing accessible.
What's the difference between a functional medicine blood test and a standard one?
It's not a different type of blood draw. The blood goes to the same labs. The difference is what gets ordered and how it's interpreted. A functional or optimization-focused panel includes more markers (50-80+ vs. 12-15), uses tighter optimal ranges instead of just standard reference ranges, and focuses on patterns across markers rather than looking at each number in isolation. It's the difference between asking "Am I sick?" and asking "How do I function at my best?"
References
- 1. Kraft R, Westman EC. "Fasting Insulin as a Predictor of Future Disease States." Presented at the American College of Nutrition, 2008.
- 2. Sniderman AD, et al. "Apolipoprotein B vs Low-Density Lipoprotein Cholesterol and Non-High-Density Lipoprotein Cholesterol as the Primary Measure of Apolipoprotein B Particle-Related Risk." J Am Coll Cardiol. 2022;79(12):1221-1233.
- 3. Tsimikas S, et al. "NHLBI Working Group Recommendations to Reduce Lipoprotein(a)-Mediated Risk of Cardiovascular Disease and Aortic Stenosis." J Am Coll Cardiol. 2018;71(2):177-192.
- 4. Holick MF. "The Vitamin D Deficiency Pandemic: Approaches for Diagnosis, Treatment and Prevention." Rev Endocr Metab Disord. 2017;18(2):153-165.
- 5. Travison TG, et al. "A Population-Level Decline in Serum Testosterone Levels in American Men." J Clin Endocrinol Metab. 2007;92(1):196-202.
- 6. Garber JR, et al. "Clinical Practice Guidelines for Hypothyroidism in Adults: Cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association." Thyroid. 2012;22(12):1200-1235.
- 7. Kraft R. "Hyperinsulinemia: A Unifying Theory of Chronic Disease." International College of Nutrition, 2011.
- 8. Ridker PM, et al. "C-Reactive Protein and Other Markers of Inflammation in the Prediction of Cardiovascular Disease in Women." N Engl J Med. 2000;342(12):836-843.
- 9. DiNicolantonio JJ, et al. "Subclinical Magnesium Deficiency: A Principal Driver of Cardiovascular Disease and a Public Health Crisis." Open Heart. 2018;5(1):e000668.
- 10. Bhasin S, et al. "Testosterone Therapy in Men With Hypogonadism: An Endocrine Society Clinical Practice Guideline." J Clin Endocrinol Metab. 2018;103(5):1715-1744.
READY TO SEE WHAT YOUR LABS ARE ACTUALLY TELLING YOU?
Stop guessing. Get a comprehensive panel with real interpretation, not just a printout with reference ranges. Serving Park Ridge, IL and the greater Chicago suburbs.